For more information, or to schedule an appointment for consultation or SLT cold laser glaucoma surgery at our practice, please fill out the contact form below. Dr. Jindra and the staff are more than happy to address any concerns you may have.
Dr. Lawrence F. Jindra
5 Covert Ave
Floral Park, New York 11001
United States of America
Ph / +1.516.616.1710
Glaucoma Diagnosis and Treatment
The leading cause of preventable blindness in the United States, glaucoma affects more than three million Americans. However, approximately half of these individuals don't even know they have the disease and many will be diagnosed only when it's too late to save vision. Glaucoma is called the "silent thief of sight" because there is no pain, no noticeable symptoms, and no cure. The good news is that glaucoma can be controlled and vision can be preserved if the condition is detected early. With vital insight about the health of your eyes we can assist you to successfully control this disease. Dr. Lawrence F. Jindra, a glaucoma specialist in Floral Park on Long Island, can provide you with all the information you need.
- General Glaucoma Information
- Types of Glaucoma and Treatment Options
- Glaucoma Detection and Diagnosis
- Glaucoma FAQs
- Additional Glaucoma Topics
General Glaucoma Information
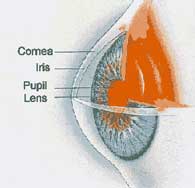 In order to understand how glaucoma develops, it is important to understand how all the parts of the eye's anterior chamber work together. The anterior chamber is a small space in the front of the eye between the cornea and the iris (the colored part of the eye). The hole in the iris is called the pupil. Behind the iris and the pupil is the lens. The anterior chamber is filled with a fluid called the aqueous humor, which brings oxygen and nutrition to the lens and cornea, and also removes waste products.
In order to understand how glaucoma develops, it is important to understand how all the parts of the eye's anterior chamber work together. The anterior chamber is a small space in the front of the eye between the cornea and the iris (the colored part of the eye). The hole in the iris is called the pupil. Behind the iris and the pupil is the lens. The anterior chamber is filled with a fluid called the aqueous humor, which brings oxygen and nutrition to the lens and cornea, and also removes waste products.
A tiny organ called the ciliary body, which is located behind the iris, continuously produces the aqueous humor. From there the aqueous flows forward through the pupil and enters the anterior chamber. Like air pumped into a tire, the aqueous keeps the eye "pumped up" to just the right pressure. The pressure inside the eye is called the intraocular pressure. The right amount of pressure depends on the correct balance of aqueous fluid going into, and the ease with which it flows out of, the anterior chamber. The aqueous humor empties out of the eye through a special drain located in the corner, or angle, where the cornea and iris meet in front of the iris. This drain is called the trabecular meshwork. The balance between the amount of aqueous fluid produced and the amount removed through the trabecular meshwork is very important. If too much aqueous is being made, if it cannot drain fast enough, or if the drain is not working properly, the pressure inside the eye will rise. The pressure in the eye can never rise so high that the eye will burst, but it can rise high enough to damage the optic nerve and cause loss of vision. This condition is called glaucoma.
Types of Glaucoma and Treatment Options
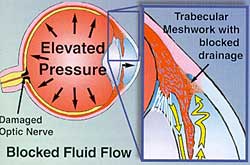 There are two basic kinds of glaucoma: open angle glaucoma and narrow angle (closure) glaucoma. In open angle glaucoma, the aqueous fluid cannot drain out of the eye properly because the trabecular meshwork is not working properly. As fluid builds up in the eye, the pressure rises. This pressure can cause irreversible damage to the optic nerve, which can lead to loss of vision. In narrow angle glaucoma, the iris root is pushed against the peripheral cornea so that the aqueous cannot even get to the drainage area of the eye. In angle closure glaucoma, this drain, the trabecular meshwork, is physically blocked by the iris. This can cause the intraocular pressure to rise dramatically and dangerously.
There are two basic kinds of glaucoma: open angle glaucoma and narrow angle (closure) glaucoma. In open angle glaucoma, the aqueous fluid cannot drain out of the eye properly because the trabecular meshwork is not working properly. As fluid builds up in the eye, the pressure rises. This pressure can cause irreversible damage to the optic nerve, which can lead to loss of vision. In narrow angle glaucoma, the iris root is pushed against the peripheral cornea so that the aqueous cannot even get to the drainage area of the eye. In angle closure glaucoma, this drain, the trabecular meshwork, is physically blocked by the iris. This can cause the intraocular pressure to rise dramatically and dangerously.
For the majority of patients with glaucoma, careful diagnosis, treatment, and long-term professional care can prevent or delay loss of vision. All patients over the age of 40 should have an eye examination that not only measures vision but also measures the intraocular pressure and examines the retina and the optic nerve every one or two years. If glaucoma is detected, several initial treatment options are available, including eye drops, oral medication, and selective laser trabeculoplasty (SLT) surgery. Depending on the type of glaucoma and other factors, one or more of these treatments may be utilized to provide safe, effective relief.
To learn more about glaucoma or to speak with Dr. Lawrence F. Jindra, a glaucoma specialist, about treatment options, contact Dr. Lawrence F. Jindra's Floral Park ophthalmology practice.
^ top
Glaucoma Detection and Diagnosis
When Dr. Jindra is trying to determine whether or not you have glaucoma, three factors will be very important: the pressure in the eye, the health of the optic nerve, and your visual field.
Intraocular Pressure
The normal intraocular pressure in the eye is between 10 and 20 millimeters of mercury. Although not everyone with intraocular pressure above 20 develops glaucoma, someone with a pressure greater than 20 is more likely to develop glaucoma. In general, the higher the pressure, the greater the chance that the patient has or will develop this condition. One of the most important facts about open angle glaucoma is that the rise in pressure inside the eye usually occurs very gradually, over a period of several months or years. Because the pressure builds up gradually, it causes no pain, redness, blurred vision, or anything else that the patient notices. Therefore, patients in the early or middle stages of open angle glaucoma have no way of knowing that they have glaucoma, unless they are examined regularly.
Optic Nerve
The next item Dr. Jindra will look at is the condition of the optic nerve. The loss of vision from glaucoma is caused by high intraocular pressure which damages the optic nerve; once vision is lost it cannot be restored. All of the current glaucoma treatment options are aimed at stopping or slowing the loss of vision by lowering the pressure in the eye. The optic nerve in patients with glaucoma is generally paler than the normal optic nerve. As glaucoma progresses, the optic nerve becomes more and more pale. Also, the optic nerve is normally mildly indented or slightly cupped. In patients with glaucoma, the indentation or cupping gets wider and deeper.
Visual Field
Loss of vision from glaucoma commonly begins in the peripheral or side vision, and then starts as tiny patches of dimness. Central vision, what we see when we are looking straight at an object, is usually not affected until late in the course of open angle glaucoma. Unfortunately, a tremendous amount of peripheral or side vision can be lost before the patient notices that anything is wrong. By the time the central vision is affected, and the patient notices the loss of vision, the glaucoma may be very far advanced and it may be very difficult to prevent further loss of vision. Dr. Jindra will test your vision to see whether there is any measurable loss of vision by doing a visual field examination. The visual field examination will test the patient's peripheral vision. The goal is to see if there are areas where the peripheral vision has already been lost. There are certain types of peripheral vision loss that are characteristic of early glaucoma. A careful visual field examination can often find this type of loss long before the patient ever notices it. If loss of vision related to glaucoma is found, Dr. Jindra will probably begin treatment to lower the pressure inside the eye. A visual field examination can be rather tedious, sometimes taking as much as several minutes per eye, but it is the best test to determine if your vision has been affected by the intraocular pressure. Regular visual field examinations are an essential part of detecting and managing glaucoma.
Diagnosis
High pressure, optic nerve damage, or reduced visual field can occur in a patient who does not, in fact, have glaucoma. But when two or three or these conditions are present in the same person, the diagnosis of glaucoma becomes more likely. In advanced cases of glaucoma the pressure inside the eye can be quite high, and there is a significant loss of tissue in the optic nerve, as well as loss of peripheral vision. Remember that in open angle glaucoma the patient can have all of these conditions for many, many years before he or she notices anything or feels that something is wrong. In angle closure glaucoma, on the other hand, the patient generally feels or notices the problem at the very beginning of the disease. The patient has a red, painful eye and will see a halo around lights and will experience a profound loss of vision within hours of the beginning of an angle closure glaucoma attack. When Dr. Jindra examines the eye, the intraocular pressure will be very high, the cornea will be cloudy, and the anterior chamber drainage angle will be blocked by the iris. Prompt diagnosis and urgent treatment is required. Angle closure glaucoma will be discussed further.
^ top
To learn more about glaucoma or to speak with Dr. Jindra about glaucoma treatment options, contact Dr. Lawrence F. Jindra's Floral Park ophthalmology practice.
Additional Glaucoma Topics
Below you will find additional information on glaucoma treatment options. Glaucoma specialist Dr. Jindra can answer any other questions you may have about glaucoma during your personal consultation at our Floral Park ophthalmology center.
- Glaucoma Check-up
- Open Angle Glaucoma
- Narrow Angle Glaucoma
- Laser Trabeculoplasty
- Laser Iridotomy
- Nerve Fiber Analysis
- Stereoscopic Disc Photos
- Blood-Flow Analysis
- Visual Evoked Potential
^ top
For more information on glaucoma treatment options, contact Dr. Lawrence F. Jindra's Floral Park ophthalmology practice.
Glaucoma FAQs
- Why do I have glaucoma?
- How did I get glaucoma?
- Do I have to watch my diet?
- Can I take hay fever medications?
- How does my blood pressure affect my glaucoma?
- Does stress or tension cause the intraocular pressure to go up?
- Will I be able to feel it when my pressure is high?
- Are cataracts and glaucoma similar or related?
- How will glaucoma eye drops affect my vision?
- Will eye drops, glaucoma laser surgery, or conventional glaucoma surgery improve my vision?
- Will I have pain during or after SLT glaucoma cold laser surgery?
- What if the SLT glaucoma cold laser surgery doesn't work?
- Will I have pain from my glaucoma surgery?
- Is glaucoma surgery safe?
- What if glaucoma surgery doesn't work?
- If I have glaucoma does that mean that I will eventually go blind?
- After my laser or conventional glaucoma surgery, will I still need the glaucoma drops?
- Is there a permanent cure for glaucoma?
Why do I have glaucoma?
Only about one in twenty cases of glaucoma in the United States is caused by an identifiable condition or event. In 95 percent of cases, glaucoma is "primary," meaning that we cannot determine its cause.
< back
How did I get glaucoma?
Unless you had a specific injury or disease, you were simply born with a tendency to develop glaucoma, and it has developed progressively throughout your life.
< back
Do I have to watch my diet?
There is no good evidence that any particular diet has an influence on glaucoma. For many reasons, a normal, balanced diet is encouraged.
< back
Can I take hay fever medications?
Many medicines for hay fever carry warnings about use by patients with glaucoma. These warnings refer to patients with untreated narrow angle glaucoma, and for the most part do not apply to patients with open angle glaucoma (or patients who have had peripheral iridectomies for their angle closure glaucoma). Make sure to inform Dr. Jindra about all your medications.
< back
How does my blood pressure affect my glaucoma?
Although uncontrolled high blood pressure can damage the vessels that supply the optic nerve, high blood pressure itself is not considered a direct cause of glaucoma.
< back
Does stress or tension cause the intraocular pressure to go up?
For the most part, how you feel or what you're doing does not affect the intraocular pressure.
< back
Will I be able to feel it when my pressure is high?
Some people say that they can feel when their pressure goes up. Although this may be true in some very unusual cases, it is not the rule. One of the main reasons glaucoma can be such a dangerous disease is that there is no way to feel the disease while it is destroying your vision.
< back
Are cataracts and glaucoma similar or related?
Cataracts (a clouding of the lens) and glaucoma are both diseases that tend to occur more in older individuals, and they both affect the front of the eye. There are many patients who have cataracts and glaucoma at the same time. With rare exceptions, however, cataracts and glaucoma are not related.
< back
How will glaucoma eye drops affect my vision?
Many drops have no affect on vision. Some glaucoma drops, such as pilocarpine, tend to affect the vision in particular patients. When you are given drops for glaucoma treatment, Dr. Jindra will check to see if they lower the pressure, if they affect your vision, and if there are any undesirable side effects.
< back
Will eye drops, glaucoma laser surgery, or conventional glaucoma surgery improve my vision?
Treatment for glaucoma rarely, if ever, improves vision. The goal of glaucoma treatment is to lower the intraocular pressure and prevent further loss of vision. No treatment can restore vision once it has been lost because of glaucoma.
< back
Will I have pain during or after SLT glaucoma cold laser surgery?
Some patients report a mild tapping or stinging sensation for a split second during SLT glaucoma cold laser surgery, but most patients feel nothing. In some, the laser causes inflammation that may make the eye a bit irritated for a day or two after SLT glaucoma laser surgery. Acetaminophen usually relieves the discomfort. This irritation is usually not severe.
< back
What if the SLT glaucoma cold laser surgery doesn't work?
We perform SLT glaucoma laser surgery at our Floral Park, Long Island office. In many cases it is as initial (primary) therapy and sometimes it is as adjunct (secondary) therapy because the medication did not adequately control the glaucoma and or the medication side effects were uncomfortable for the patient. If SLT glaucoma laser surgery does not work, resuming medication may help. If not, conventional glaucoma surgery may be advised.
< back
Will I have pain from my glaucoma surgery?
There may be some mild pain in the first few days after glaucoma surgery. Severe or debilitating pain is extremely rare. Also, during the first few days or weeks after glaucoma surgery, the eye may not see quite as well as it did before the surgery.
< back
Is glaucoma surgery safe?
All surgery carries some risks. Glaucoma surgery is no exception. Sometimes further loss of vision may occur. It is important to remember that in some cases, the surgery may not work to control the glaucoma. Dr. Jindra will explain all of the risks and benefits of glaucoma surgery.
< back
What if glaucoma surgery doesn't work?
Glaucoma surgery is delicate and requires precise healing. Fifteen to 20 percent of glaucoma surgeries are not successful. Most of the failures occur because the healing process cannot be controlled perfectly. If there is too much healing, the opening closes up, and the pressure goes up. If there is not enough healing, and the drain is letting too much fluid out, the pressure may drop too low. Sometimes it may be necessary to continue glaucoma medication after surgery. If the glaucoma is still not controlled, another operation may be advised.
< back
If I have glaucoma does that mean that I will eventually go blind?
The vast majority of patients with open angle glaucoma retain good vision for their lifetime. However, in some cases, even with the best treatment, glaucoma cannot be controlled and may cause lose of vision and even blindness.
< back
After my laser or conventional glaucoma surgery, will I still need the glaucoma drops?
Approximately one out of four patients can stop using eye drops after glaucoma laser surgery. About half of those who have filtering surgery for glaucoma can stop using drops.
< back
Is there a permanent cure for glaucoma?
Generally, there is no permanent cure for glaucoma. In some patients, glaucoma surgery can reduce the intraocular pressure to normal levels without medicines indefinitely. It is important for all patients with glaucoma to continue a lifelong program of regular visits to the office of Dr. Jindra to make sure that the glaucoma stays under control.
< back
To learn more about glaucoma and SLT glaucoma cold laser surgery, contact Dr. Lawrence F. Jindra's Floral Park ophthalmology practice.
^ top